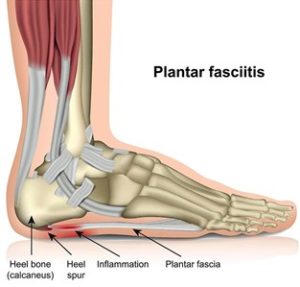
Heel pain is often caused by plantar fasciitis – an inflammation of the large tissue band (plantar fascia) connecting the heel bone to the toes.
The pain is usually felt under the heel and symptoms can vary from sharp, dull, ache, burning sensation and sometimes mild swelling.
The research tells us that many people aren’t able to manage this condition effectively on their own. However, asking the right questions is key to the resolution.
- Plantar heel pain is a common problem. 4% of adults have it at any given point in time. [1] This increases to 10% in those over 50. [2]
- It can hang around longer than you might like. Research indicates up to 80% of patients still report symptoms at 1 year, and 50% at 5 years. [3]
Is it plantar fasciitis?
 Most often, yes, but when it’s not the management can be very different. Heel fat pad irritation is another condition that presents very similarly, but may need a slightly different approach.
Most often, yes, but when it’s not the management can be very different. Heel fat pad irritation is another condition that presents very similarly, but may need a slightly different approach.
Nerve irritations, bone stress injuries, and more nasty masquerading conditions need different investigations and advice.
Often quicker assessments brush over these possibilities, so it’s worth having an experienced musculoskeletal physiotherapist to assess your condition.
Determining the cause of the problem involves considering the risk factors and the size of their influence. In a physiotherapy assessment we look for:
- A pattern of overload – where there is a large increase in what you do on your feet, relative to what you’ve been doing;
- Signs of a systemic cause – such as an underlying inflammatory condition; and
- Biomechanical explanations – for increased plantar loads (weight, lower limb and foot mechanics).
What treatment works best?
Your treatment plan is based on your individualised assessment. There is also a breadth of research we utilise, to understand what works, how much and how long for.
When comparing different methods, there isn’t one type of management that stands out as most helpful, which points us back to an individualised plan based on your presentation and preferences.
There is one certainty we recommend: The foundation for improvement is understanding what capacity those painful tissues have for tolerating what they are being asked to do.
Failing to answer this question can lead to a long and frustrating road!
What about trying………..?
You’ve probably come across some options through internet searches and your social circles and it’s hard to know what to expect!
After spending months immersed in plantar fasciitis reading and writing, being involved in research and exploring people’s experiences with their many treatment options for plantar fasciitis, I’ve listed a brief summary:
Manual therapy
Release work to the calf and foot seem more helpful than joint techniques and are best used in combination with a more active approach. Anecdotally, many patients find this helpful but it seems only one piece of the puzzle.
Medication
Anti-inflammatories widely recommended, but the real effect is probably quite small and not much better than placebo. It is better to think about the driving causes, not just managing the symptoms.
Weight loss
The most significant risk factor and addressing this for the long-term is likely to have significant benefit.
Taping
Helpful for most to unload the area but not to be relied on as a long-term solution.
Orthotics
Helps for many. Research indicates a custom orthotic doesn’t seem to be more effective than something off the shelf.
Shoes
Although probably not the sole cause of the problem, changing these can impact things by altering the mechanics of the foot and therefore could be an approach that helps.
Strengthening exercises
Specific exercises can toughen up your plantar fascia and create a stronger support structure in your foot. This method has a significant effect over the long-term. It is often neglected but seems to help where other avenues fail.
Injections
Combining all the studies together, we see that injecting a steroid is better than a placebo injection. However, the size of this effect is small and short lived. It’s important to weigh the risks and benefits as multiple injections can be harmful for tendons long term.
Shockwave
A new modality, which the research indicates might be effective. It can be painful and is usually saved until conservative options have been looked at.
Surgery
Definitely a last resort and needing a clear and specific indication for why?
As indicated from the research, this condition is multifactorial and successful management depends on answering a few key questions first!
If you need help with heel pain and getting back to doing what you enjoy in life, please get in touch.
Alex Flood – Musculoskeletal Physiotherapist
References:
1 Hill CL, Gill TK, Menz HB, et al.Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. J Foot Ankle Res2008;1:2.
2 Roddy E, Case R, Thomas MJ, et al.Population prevalence and associations of plantar heel pain in adults aged 50 years and over: cross-sectional findings from the Clinical Assessment Study of the Foot. 2015;54:39–40.
3 Hansen L, Krogh TP, Ellingsen T, et al.Long-Term Prognosis of Plantar Fasciitis: A 5- to 15-Year Follow-up Study of 174 Patients With Ultrasound Examination. Orthop J Sports Med2018;6:2325967118757983.